When it comes to pharmacovigilance, many people may think it’s the responsibility of finished drug manufacturers or regulatory agencies, and has little to do with API production.
However, the opposite is true—fluctuations in API quality, changes in impurity profiles, and even adjustments to the synthesis route can directly impact the safety of the final drug. Today, I’ll discuss what pharmacovigilance is and why it’s so crucial for API companies, from a frontline perspective.
Does Pharmacovigilance Equal Drug Safety? It’s Actually a “Dynamic Safety Firewall”
The official definition of pharmacovigilance (according to the WHO) is: “The science and practice of monitoring, evaluating, understanding, and preventing adverse drug reactions and any other potential drug-related problems.”
Sounds abstract? To put it simply, it’s a 24/7 drug safety monitoring system designed not only to detect adverse reactions after they occur, but also to prevent them before they occur.
Pharmacovigilance is particularly important for API companies:
Genotoxic impurities (such as nitrosamines), unknown impurities, and changes in crystalline form in APIs can all potentially trigger safety signals.
Changes in synthesis processes and adjustments to starting material sources require a risk reassessment based on pharmacovigilance data.
Drug regulatory authorities (such as the FDA and EMA) have significantly strengthened pharmacovigilance requirements for API companies in recent years, and audits often examine the robustness of relevant systems.
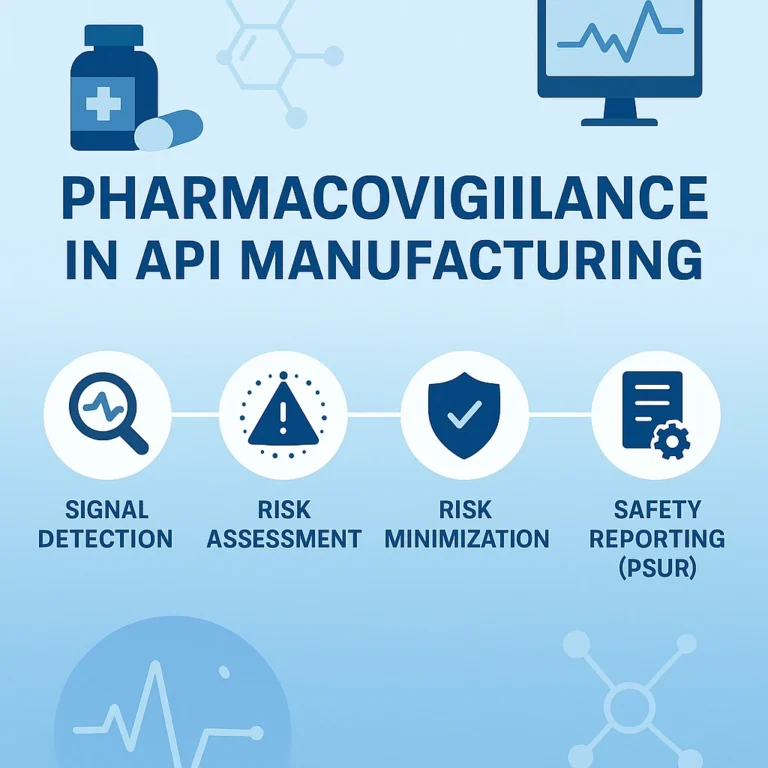
How Does Pharmacovigilance Actually Work? Four Core Steps from Reporting to Action
Many people think pharmacovigilance is simply about collecting adverse reaction reports, but it is actually a closed-loop management system that primarily includes:
- Signal Monitoring and Collection
Sources: This includes not only adverse drug reaction (ADR) reports from medical institutions, but also literature, social media, and even discussions on patient forums.
Our role as API companies: If a batch of intermediates or API is found to pose a potential risk (such as the detection of a new trace impurity), we must proactively notify downstream pharmaceutical manufacturers.
- Risk Assessment and Analysis
Methods: Statistical and epidemiological methods are used to determine whether the association between an adverse event and the drug is accidental or causal.
Typical scenario: Nitrosamine impurities are detected in an antihypertensive drug → The pharmacovigilance team needs to assess: What is the carcinogenic risk at different concentrations? Which batches are affected? Should a recall be required?
- Risk Minimization Actions
Measures: Modify drug inserts, issue medication warnings, restrict the intended use, or even recall or withdraw the product.
Drug API Level Interaction: If the risk is determined to be due to a specific impurity in the API, immediate optimization of the synthesis process and strengthening of purification controls are required.
- Periodic Safety Update Report (PSUR)
Requirement: Pharmaceutical companies must submit PSURs to drug regulatory authorities on a regular basis (e.g., semi-annually), summarizing all safety data collected during the period and providing conclusions.
Drug API companies must also provide: process change records, impurity profile data, stability test results, etc.